Patrick O’Farrell, the pre-eminent historian of the Irish and the Catholic Church in Australia and New Zealand, was long associated with the University of New South Wales, arriving in 1959 ten years after it had been founded as Sydney’s second university. Originally ‘The New South Wales University of Technology’, it grew out of Sydney Technical College, expanding rapidly in the 1950s and 60s:
The commencement of medicine in 1961 was, of course, a major extension of the university’s persona. But it was not until its actual establishment that the university fully realised how costly it was, particularly in relation to teaching hospitals, and this
in a university already, because of its scientific and technological nature, a high cost academic environment. The initial teaching hospitals were Prince Henry at Little Bay and Prince of Wales at Randwick, with specialised arrangements with some other metropolitan hospitals. For the first time in Australia clinical professors in the university medical school were directors of the clinical departments in the teaching hospitals. At every point in this enterprise there was criticism and contention, professional and public. The queen’s opening of the first building, in 1963, went forward with due pomp and apparent tranquillity, but in fact it was not until 1967 that the university itself felt relatively easy about its medical financing and teaching hospital provision.
Even by 1965 Medicine had gained an attractive reputation amongst those students not constrained by family traditions dictating continuance at the University of Sydney. And it offered advantages in other ways. If you took Maths as an option, and decided doctoring was not for you, you could transfer to Science, even Engineering at the end of first year. University of New South Wales courses were acquiring a superior reputation among informed parents by the 1970s. To a student reminiscing of entering in 1965 (won over by the Open Day comparisons), Sydney seemed entrenched in tradition, behind the scientific times. The University of New South Wales seemed new, with excellent teachers, much better equipment, and much more ‘modern’ in its attitude towards the science of the time. Experience in the medical school confirmed this. And also an atmosphere of happy harmony between students – male and female; impressionistically one-third Jewish, one-third ‘average Australians’, one-third Asian – with a staff significantly Catholic. Or so it was believed, though precise actualities suggest perhaps otherwise. Is it also apocryphal that at the Roundhouse medical ball in 1964 a professor stripped naked and danced around on the table? As in all medical matters, stories abound. As also in matters of students living very hard, experimenting with drugs, magic mushrooms, and the like. What seems to be the case, however, is a certain degree of pro-doctor prejudice among staff, who tended to anticipate in students a medical family background and a private school education. Correctly, by and large, in that many of the students were doctors’ sons who could not get into Sydney.
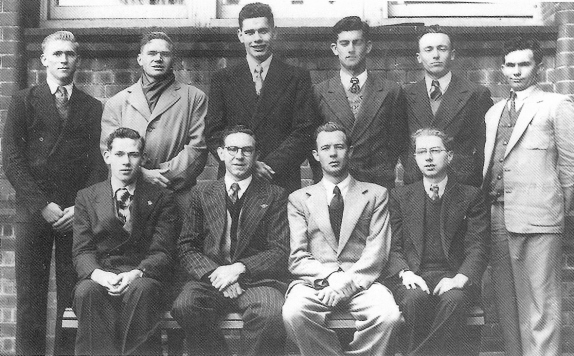
First Committee of Society of Students (forerunner to Students’ Union), including my father Bob Morgan standing third from left, 1951 (GK Cranny/UNSW Archives Collection)
So what? Medical students at the University of New South Wales were well aware of their superior facilities – for instance, four to a cadaver as against around thirty at Sydney, where facilities were ‘grim’. Those in a position to compare – in microbiology for instance – found a much closer relationship between students and tutors: in practical classes each tutor had ten or twelve students; at Sydney, thirty, with no chance to get to know students. And at the University of New South Wales the emphasis was on modern teaching methods – defining goals and what to know to get there. Set against this was the faculty’s policy for choosing the better students from first year Science at the cost of excluding their own bottom students, a practice which raised some vigorous parental objection. Even among staff there were those who protested, to the point of resignation, against the severity of standards. Indeed they were severe: anatomy and obstetrics held weekly examinations; other subjects demanded large ‘holiday’ tasks, physiology for instance. At the University of New South Wales determination to be equal to the best sometimes took it too far. The government was to intervene to allow more students to progress – leading to staff protest. And internal rumpus – the first professor of Physiology resigning in conflict with the dean, Rundle. Of the 117 who enrolled in the second intake in medicine, 26 reached the finals in December 1967. Over 75 per cent of the Class of 1968 were in specialty positions thirty years later. The student costs at university amounted to fatigue and some feeling of deprivation that there was not sufficient time to grow and enjoy university life. In fact, in the clinical years the system and requirements of the course meant living in, in a variety of hospitals – little time or opportunity for ‘university life’.
There was some professional resistance to this new wave of intensive training. The 1950s and 1960s were dominated by anecdotal as against evidence-based medicine. Thus, there was some antipathy to academic, science-oriented medicine among general practitioners and hospitals – and it was there that the emphasis of the teaching of medicine at the University of New South Wales lay. However, the faculty had the initial advantage of hard men in charge, first-rate men of great ability and reputation, but, above all, deciders, autocrats with it – master builders of a new, complex, medical edifice. Within the rules of the institution, though. Evolved from public service and Sydney Technical College backgrounds was a rigid teaching hourage requirement: at the top, tutors around sixteen hours a week; graduating down to professors at four to six hours, with allowance for evening classes. Strict adherence to this was the basic requirement for any argument for
additional staff. Medicine was no exception to this rule. The university’s reputation for hard-working teachers in all faculties sprang in part from youth and commitment but also from this simple measure of coercion.
As to Medicine, a major influence was the relationship (if that is the right word) with Sydney University: dead hostile initially to the University of New South Wales medical school; then anger, resentment, regret, and finally acceptance – though not without using its old boys’ network to secure the new Westmead Hospital in the 1970s, and attempting to outstrip the University of New South Wales in its decision to introduce the five-year degree in 1973-74 (the six-year course came back in 1988). Medical politics tended to be petty, competitive, and nasty: in no area did the University of Sydney-University of New South Wales rivalry last longer, or be as intense, as in medicine. Meanwhile, John Hickey and Doug Tracy were putting St Vincent’s ahead on the medical map. And major developments focussed on Prince of Wales, to make it the major hospital it is today.
At the University of New South Wales were lateral-thinking, teaching doctors, destined to be leaders in their fields: Penny, Dwyer, Hollows, Beveridge, McCloskey, and so on – men who did not wish to stay with the establishment, but to create and mould a new medical world of their own. As human beings. Their attitude to patients – listen, talk – was very different from the superiority affected by Sydney. At that early stage, entry was not determined by an astronomical, competitive Tertiary Entrance Rank (TER) performance, a situation of requirement which many medical staff were to deplore: students offering no people skills, indeed anything beyond being good at getting marks.
-Patrick O’Farrell, New Zealander-Australian, 1933-2003

